|
https://www.ncbi.nlm.nih.gov/pubmed/24459197
Clinical update
Central blood pressure:
current evidence
and clinical importance
Carmel M. McEniery1*,
John R. Cockcroft2,
Mary J. Roman3,
Stanley S. Franklin4, and Ian B.Wilkinson1
1Clinical Pharmacology Unit,
University of Cambridge, Addenbrooke’s Hospital, Box 110, Cambridge CB22QQ, UK; 2Department of Cardiology,Wales Heart Research Institute, Cardiff
CF14 4XN, UK; 3Division of Cardiology,Weill Cornell Medical College, New York, NY 10021,
USA; and 4University of California, UCI School of Medicine, Irvine, CA 92697-4101,
USA
Received 29 April 2013; revised 27 November
2013; accepted 17 December 2013; online publish-ahead-of-print 23 January 2014
and central pressure. Therefore, basing
treatment decisions on central, rather than brachial pressure, is likely to
have important implications
for the future diagnosis and management of
hypertension. Such a paradigm shift will, however, require further, direct
evidence that selectively
targeting central pressure, brings added
benefit, over and above that already provided by brachial artery pressure.
Central pressure † Blood pressure † Anti-hypertensive treatment † Cardiovascular risk
Introduction
The brachial cuff sphygmomanometer was
introduced into medical
practice well over 100 years ago, enabling
the routine, non-invasive,
measurement of arterial blood pressure. Life
insurance companies
were among the first to capitalize on the
information provided by
cuff sphygmomanometry, by observing that
blood pressure in
largely asymptomatic individuals relates to
future cardiovascular
risk—observations that are nowsupported by a wealth of epidemiological
data.1 The most recent Global Burden of Disease report2
identified hypertension as the leading cause
of death and disability
worldwide. Moreover, data from over 50 years
of randomized controlled
trials clearly demonstrate that lowering
brachial pressure,
in hypertensive individuals, substantially
reduces cardiovascular
events.1,3 For these reasons, measurement of brachial blood pressure
has become embedded in routine clinical
assessment throughout the
developed world, and is one of the most
widely accepted ‘surrogate
measures’ for regulatory bodies.
The major driving force for the continued use
of brachial blood
pressure has been its ease of measurement,
and the wide variety of
devices available for clinical use. However,
we have known for over
half a century that brachial pressure is a
poor surrogate for aortic
pressure, which is invariably lower than
corresponding brachial
values. Recent evidence suggests that central
pressure is also more
strongly related to future cardiovascular
events4 – 7 than brachial
pressure, and responds differently to certain
drugs.8,9 Appreciating
this provides an ideal framework for
understanding the much publicized
inferiority of atenolol and some other
beta-blockers,10 compared
with other drug classes, in the management of
essential
hypertension. Although central pressure can
now be assessed noninvasively
with the same ease as brachial pressure,
clinicians are unlikely
to discard the brachial cuff sphygmomanometer
without
robust evidence that cardiovascular risk
stratification, and monitoring
response to therapy, are better when based on
central rather
than peripheral pressure. Central pressure
assessment and accuracy
will also have to be standardized, as it has
been for brachial pressure
assessment with oscillometric devices. This
review will discuss our
current understanding about central pressure
and the evidence
required to bring blood pressure measurement,
and cardiovascular
risk assessment into the modern era.
Physiological concepts
Arterial pressure varies continuously over
the cardiac cycle, but in
clinical practice only systolic and diastolic
pressures are routinely
reported. These are invariably measured in
the brachial artery
using cuff sphygmomanometry—a practice that has changed
little
over the last century. However, the shape of
the pressure waveform
* Corresponding author. Tel: +44 1223 336806, Fax: +44 1223
216893, Email: cmm41@cam.ac.uk
Published on behalf of the European Society
of Cardiology. All rights reserved. &The Author
2014. For permissions please email: journals.permissions@oup.com
European Heart Journal (2014) 35, 1719–1725 doi:10.1093/eurheartj/eht565
Pressure measured with a cuff and
sphygmomanometer in the brachial artery is accepted as an important predictor
of future cardiovascular risk.However, systolic pressure varies throughout the
arterial tree, such that aortic (central) systolic pressure is actually lower
than corresponding brachial values, although this difference is highly
variable between individuals. Emerging evidence now suggests that central
pressure is better related to future cardiovascular
events than is brachial pressure. Moreover, anti-hypertensive drugs can exert
differential effects on brachial and central pressure.
Therefore, basing treatment decisions on central, rather than brachial
pressure, is likely to have important implications for
the future diagnosis and management of hypertension. Such a paradigm shift
will, however, require further, direct evidence that selectively targeting central pressure, brings added benefit, over and above
that already provided by brachial artery pressure.As discussed earlier, a full
synthesis of the available evidence concerning
central pressure and the risk of future
cardiovascular events is now required. However, it will also be necessary to
determine the clinical relevance of differences between
brachial and central pressure
for the individual patient, especially given
the relatively high correlation between the two. Emerging
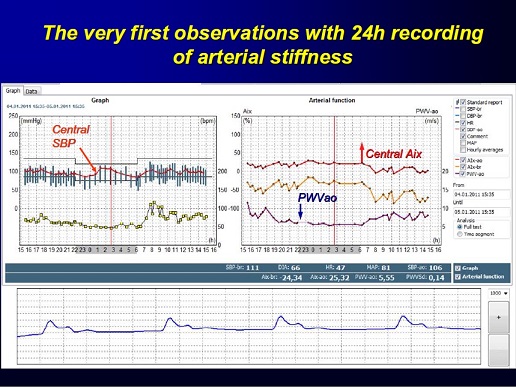
data support the prognostic superiority of both 24-h
ambulatory blood pressure monitoring
(ABPM)79 – 81 andhomemonitoring81 in
comparison with office measurements. Interestingly,
a recent study82 demonstrated that 24-h ambulatory cuff pressures were comparable with office central pressure
measurements in the prediction of risk,
although the significance of this study awaits confirmation.83 As yet, there are no data comparing the
predictive value ofhomemonitoring vs. central pressure in the
prediction of risk. Ultimately, it will be
necessary to evaluate the prognostic value of 24-h
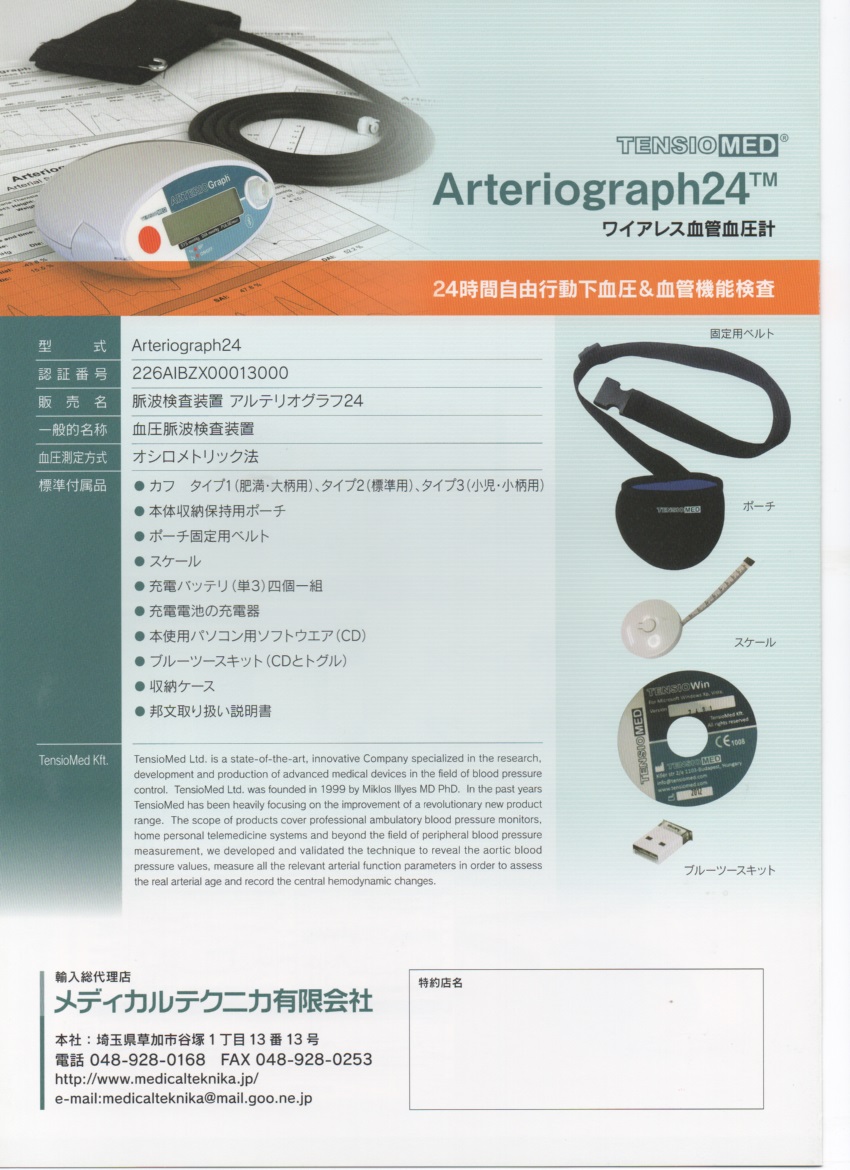
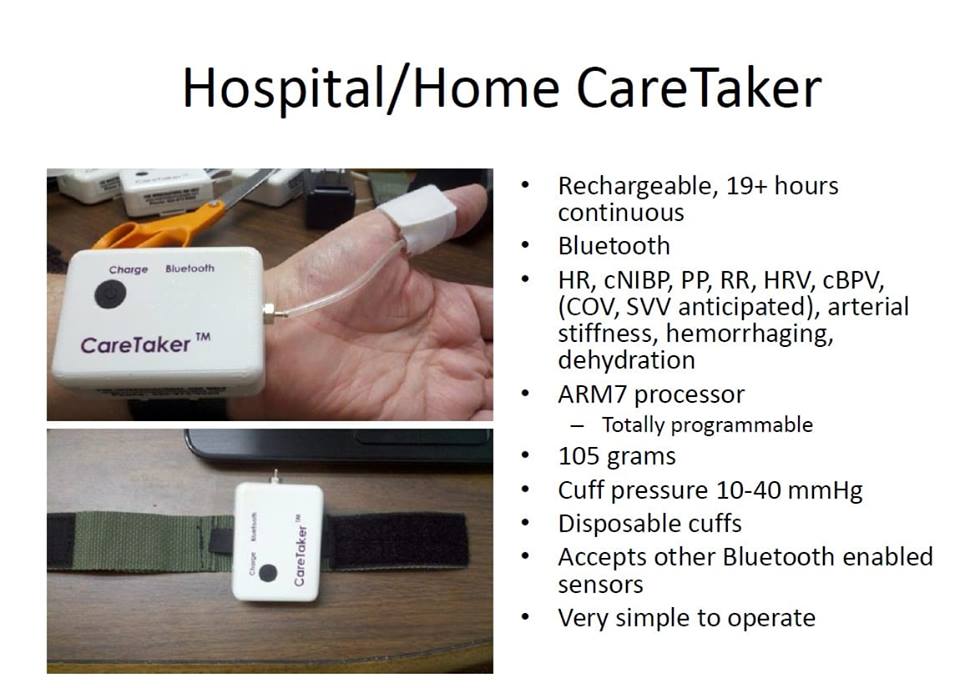
ambulatory central pressure.With the recent development of ambulatory central pressure systems,84,85 this is now
possible and it may be reasonable to
hypothesize that 24-h central, rather than brachial ABPM
would be superior in terms of risk prediction.
|