|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
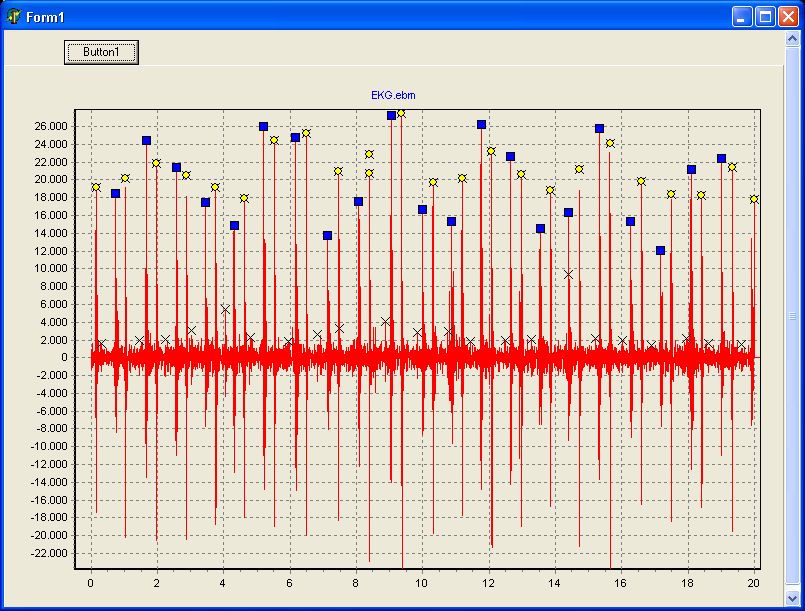
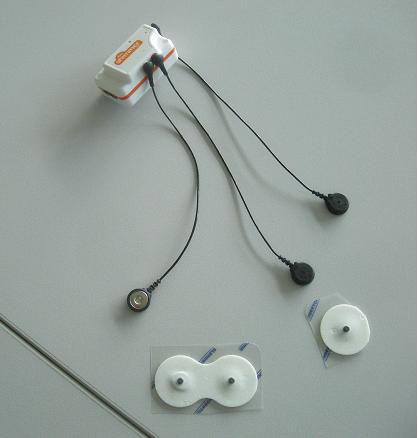
ViScope100 聴診音が、その計測部のダイヤフラムの部分に連続表示されます。 また、SDカードに記憶されたデータは専用ソフトウエアでパソコンに表示記憶できます。 |
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
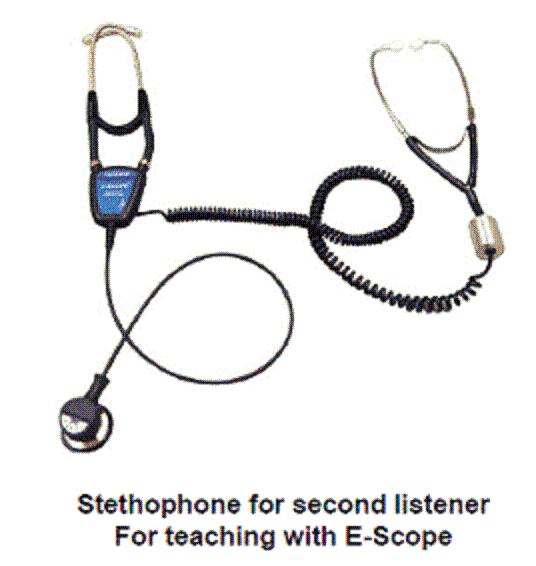
1. 聴診音の教育用として、 電子ヘッドホンを多数の生徒が同時に聞くことができる。 電波距離約10mで、電子聴診器部で送信ボタンを押す 2.iPhone でも聴診音を受信・音声聴診できる 3.電子カルテなどのソフトウエアへ送信できる 4.ペットの処置等に、ペットの心音をモニターできる 5.標準二分間稼動するが、一時間まで設定を変えることができる 6.耳が不自由な医療従事者に、有効なツールとして採用頂く 7.歯科医師等の歯科処置中に、患者の心音又は呼吸音をモニターできる 8.危険物・有害物を扱う場面での有効なモニター方法を提供する 9.救命救急時の、救急車中などの用途として役立つ. 10、スポーツ、リハビリ、在宅看護、山間部、 離島などの遠隔監視用として有効 |
||||||||||||||||||||||||||||||||||
iPod, iPad, iPhone 等による 聴診音の リアルタイム 連続波 表示、記憶、記録、他へ転送、が安い価格で可能となりました。 、 |
||||||||||||||||||||||||||||||||||
当カルディオニクス社製シミュレータについては、 概要を下記にてご案内しております。 各種シミュレータはこちら 販売を希望される会社を募集 |
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
iPod, iPad, iPhone 等に、画像化表示するシステムをご案内します。 其の他、お問い合わせ下さい。
http://www.din.or.jp/~meditekn/medi_hp/ |
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
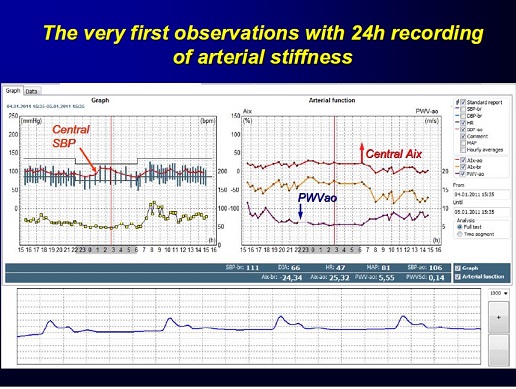
https://www.ncbi.nlm.nih.gov/pubmed/24459197 Clinical update Central blood pressure: current evidence and clinical importance Carmel M. McEniery1*, John R. Cockcroft2, Mary J. Roman3, Stanley S. Franklin4, and Ian B.Wilkinson1 1Clinical
Pharmacology Unit, University of Cambridge, Addenbrooke’s
Hospital, Box 110, Cambridge CB22QQ, UK; 2Department of Cardiology,Wales Heart Research Institute,
Cardiff CF14 4XN, UK; 3Division
of Cardiology,Weill Cornell Medical College, New York, NY 10021, USA; and 4University of California, UCI School of
Medicine, Irvine, CA 92697-4101, USA Received 29 April 2013;
revised 27 November 2013; accepted 17 December 2013; online
publish-ahead-of-print 23 January 2014 and central pressure. Therefore, basing treatment decisions on central,
rather than brachial pressure, is likely to have important implications for the future diagnosis and management of hypertension. Such a paradigm
shift will, however, require further, direct evidence that selectively targeting central pressure, brings added benefit, over and above that
already provided by brachial artery pressure. Central pressure † Blood pressure † Anti-hypertensive treatment † Cardiovascular risk Introduction The brachial cuff sphygmomanometer was introduced into medical practice well over 100 years ago, enabling the routine, non-invasive, measurement of arterial blood pressure. Life insurance companies were among the first to capitalize on the information provided by cuff sphygmomanometry, by observing that blood pressure in largely asymptomatic individuals relates to future cardiovascular risk—observations that are nowsupported by a wealth of
epidemiological data.1 The most recent Global Burden
of Disease report2 identified hypertension as the leading cause of death and disability worldwide. Moreover, data from over 50 years of randomized controlled trials clearly demonstrate that lowering brachial pressure, in hypertensive individuals, substantially reduces cardiovascular events.1,3 For these reasons, measurement of brachial blood pressure has become embedded in routine clinical assessment throughout the developed world, and is one of the most widely accepted ‘surrogate measures’ for regulatory bodies. The major driving force for the continued use of brachial blood pressure has been its ease of measurement, and the wide variety of devices available for clinical use. However, we have known for over half a century that brachial pressure is a poor surrogate for aortic pressure, which is invariably lower than corresponding brachial values. Recent evidence suggests that central pressure is also more strongly related to future cardiovascular events4 – 7 than brachial pressure, and responds differently to certain drugs.8,9 Appreciating this provides an ideal framework for understanding the much publicized inferiority of atenolol and some other beta-blockers,10 compared with other drug classes, in the management of essential hypertension. Although central pressure can now be assessed noninvasively with the same ease as brachial pressure, clinicians are unlikely to discard the brachial cuff sphygmomanometer without robust evidence that cardiovascular risk stratification, and monitoring response to therapy, are better when based on central rather than peripheral pressure. Central pressure assessment and accuracy will also have to be standardized, as it has been for brachial pressure assessment with oscillometric devices. This review will discuss our current understanding about central pressure and the evidence required to bring blood pressure measurement, and cardiovascular risk assessment into the modern era. Physiological concepts Arterial pressure varies continuously over the cardiac cycle, but in clinical practice only systolic and diastolic pressures are routinely reported. These are invariably measured in the brachial artery using cuff sphygmomanometry—a practice that has changed
little over the last century. However, the shape of the pressure waveform * Corresponding
author. Tel: +44 1223 336806, Fax: +44 1223 216893, Email: cmm41@cam.ac.uk Published on behalf of the European Society of Cardiology. All rights
reserved. &The Author 2014. For
permissions please email: journals.permissions@oup.com European Heart Journal (2014) 35, 1719–1725 doi:10.1093/eurheartj/eht565 Pressure measured with a cuff and sphygmomanometer in the brachial artery
is accepted as an important predictor of future cardiovascular risk.However,
systolic pressure varies throughout the arterial tree, such that aortic
(central) systolic pressure is actually lower than corresponding brachial values, although
this difference is highly variable between individuals. Emerging evidence now
suggests that central pressure is better related to
future cardiovascular events than is brachial pressure. Moreover, anti-hypertensive
drugs can exert differential effects on brachial and
central pressure. Therefore, basing treatment decisions on central, rather than
brachial pressure, is likely to have important implications for the future diagnosis and management of hypertension. Such a
paradigm shift will, however, require further, direct evidence that selectively targeting central pressure, brings added benefit, over and above
that already provided by brachial artery pressure.As discussed earlier, a full
synthesis of the available evidence concerning central pressure and the risk of future cardiovascular events is now required. However, it
will also be necessary to determine the clinical
relevance of differences between brachial and central pressure for the individual patient, especially given the relatively high
correlation between the two. Emerging data support the prognostic superiority of both 24-h ambulatory blood pressure monitoring (ABPM)79 – 81 andhomemonitoring81 in comparison with office measurements. Interestingly, a recent
study82 demonstrated that 24-h ambulatory cuff pressures
were comparable with office central pressure measurements in the prediction of risk, although the significance of this study awaits
confirmation.83 As yet,
there are no data comparing the predictive value ofhomemonitoring vs. central
pressure in the prediction of risk. Ultimately, it will be necessary to evaluate the
prognostic value of 24-h ambulatory central pressure.With the recent
development of ambulatory central pressure systems,84,85 this is now possible and it may be reasonable to hypothesize that 24-h central, rather than brachial ABPM
would be superior in terms of risk prediction.
|
||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||